Yesterday I gingerly pulled myself up from the borrowed hospital wheel chair and stepped on the scale as protocol for my oncology check up. I was prepared to see a number that reflected my current state of frailty and weakness but I was not prepared to hear her said “okay, eighty pounds”. Honestly it scared me and I plopped back down into the wheelchair in disbelief. All I could think of is “Shit. I have a long road ahead of me.”
It’s not that a long road wasn’t glaringly apparent prior to that weigh in. It just served as a reminder that the past few months have left me beyond depleted. I am a twenty-nine year old trapped in the body of a ninety-five year old. My lungs are still surrounded by fluid, albeit less fluid than a few months ago. So my lungs need help too. Breathing fully can be a struggle, walking is a struggle, staying out of my own head is the biggest struggle.
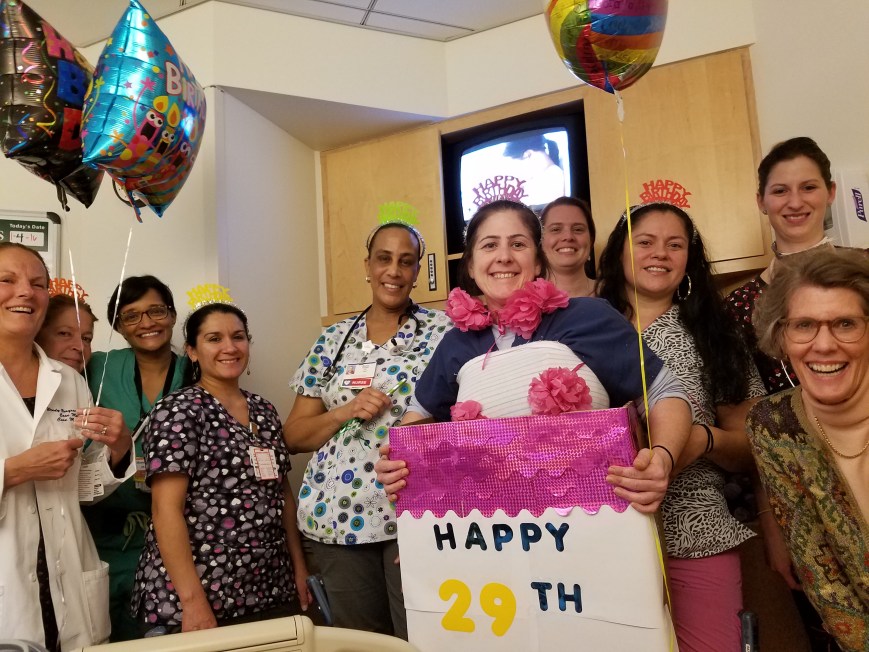
Now let’s let one thing be clear, struggles aside I am beyond thrilled to be home. I received top notch care in the hospital from all of my loving nurses, CNA’s and docs. But nothing compares to being in your own familiar space with peaceful silence and comforts unique to you. Most of all, I am just happy to be back living with Cory in this little home we have created together. Just sitting on the couch at the end of the night in front of the television. It’s comforting to turn to my left and know he’s there smiling back at me, making bad jokes, and oozing love and compassion in ways that deserve to be described in its own entry. There is no replacement for being away from your love.
There is another aspect to being home that one doesn’t think much about until you’re actually there. After two full months in bed, medicated, sedentary, catered to hand and foot being home means that you are now doing these tasks yourself. As my doctor reminded me when I was venting how hard this all is I went from zero to doing twenty times more than I have in months. These aren’t huge tasks either- walking from the living room to the kitchen. There have been times I made it to the fridge and just sat on the floor for a few minutes to recover before heading back.
I have been so fortunate to have Cory help me in all the little ways that matter and add up. He never complains. My parents have also made a special effort to be with me a couple days a week when Cory is working outside of the home all day. Not only have they helped nurture me and keep my head on straight, they also have done a tremendous amount of cleaning, organizing, and shopping to make both of our lives easier. I can’t imagine doing this by myself. If I still lived alone it would be bad news bears.
Finally- sleeping and eating. Right now I can only have clear or full liquids. As soon as something goes down my throat it just trickles back down my g-tube into a plastic “bladder” that sits beside me on the floor. Let me tell you that it is REAL strange to see your stomach contents just float by you through a tube just minutes after ingesting it. But keeping the tube open isn’t what’s going to help me gain back my weight and strength. The goal of getting rid of the g-tube will have to be taking in something like a yogurt smoothie or ensure, clamping off the g-tube so my body absorbs and processes it naturally, then staying clamped for a few hours without getting nauseous or throwing up.
Clamping is a mental game. I become too obsessed over it, how long I’ve been clamped, staring at the clock. Dr.Robison suggested doing it when I watch a movie or have some sort of distraction. Slowly but surely I will get there because even though I am grateful that it’s helping me, I HATE it and need it to be gone as a piece in the quest for modified normalcy.
Another true mental game is sleeping. I have only slept fully through the night once and I barely can nap during the day. This is no help when it comes to regaining my strength. I’m exhausted and captured by insomnia. The nights are long and to add complication, I am hooked up to a big bag of TPN AND the gtube so getting around the house when I can’t sleep is daunting to say the least. I’ve tried sleep aids and medications (assuming they stay down) but nothing seems to help. Someday I’ll regulate but for now- these are some longggg days.
So there you have it. Life at home one week out of discharge. It could be better, it could be worse.
I just need to remember everything else I have overcome in previous years, when I go to that place of defeat in my head . None of it was easy or quick and it all took work and patience. This is no different.
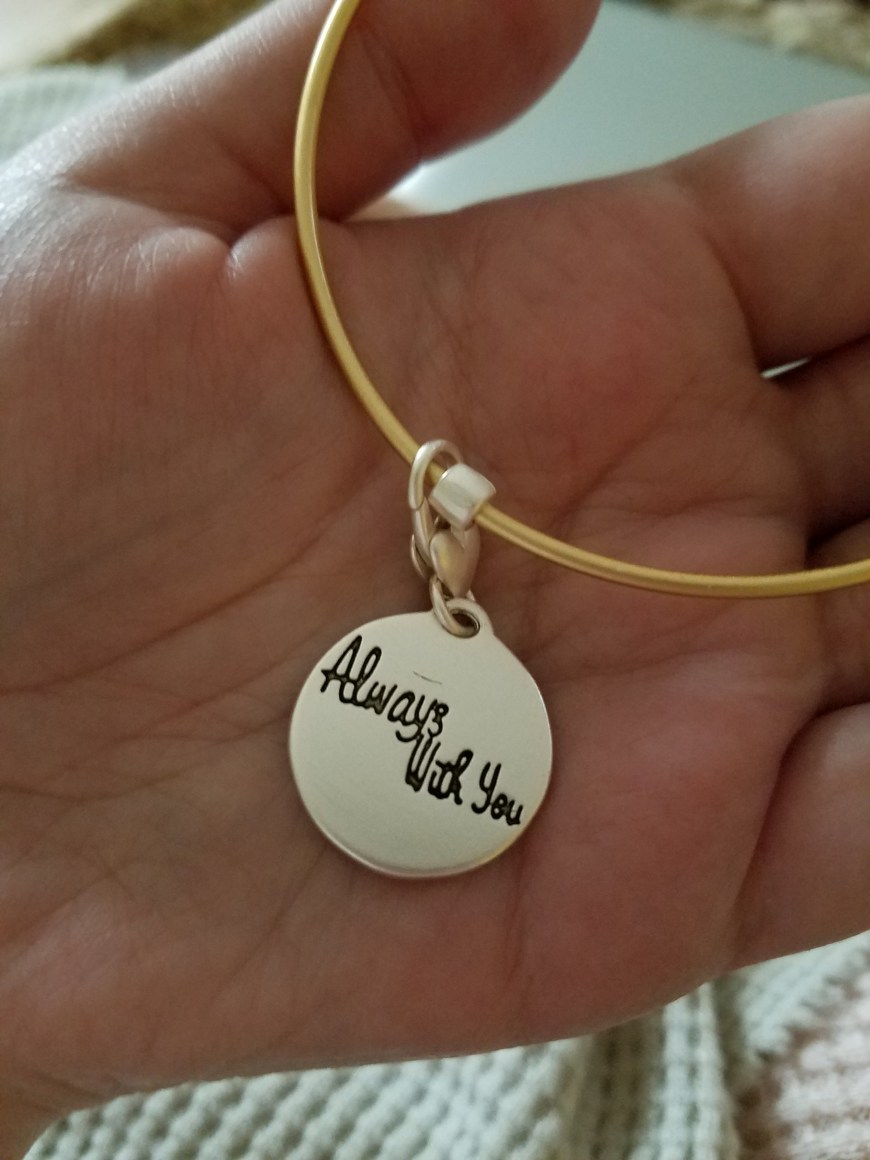
Lastly, as always I am grateful to those that have checked in on me, sent gifts, spared a kind word. It means so much to me.
So what’s next? Just adjusting to home until Feb 23rd when I see my doctor again and have my next round of chemo.
I think that’s all I can say for now. Sending love to you all.














 I was going to make a cheeky joke about the hot sauce joke from Dumb and Dumber when it dawned on me that this gif is the actual personification of my small intestine gearing up to ruin my life.
I was going to make a cheeky joke about the hot sauce joke from Dumb and Dumber when it dawned on me that this gif is the actual personification of my small intestine gearing up to ruin my life.